Why pain management is important and understanding different types of pain is crucial?

Pain management is a cornerstone in nursing care. It’s not just about giving out medications, it’s about completely understanding what the patient is suffering and providing the best treatment to reduce their discomfort. As a beginning nurse, understanding the different types of pain and the underlying mechanisms is your first vital step to provide a comprehensive assessment and appropriate treatment.
- Firstly, acute pain. Typically, acute pain acts as a loud alarm, telling something is wrong, normally after an injury, surgery, or illness. It’s sharp and short-lived, subsiding as the underlying cause heals.
- Secondly, chronic pain. This type is more like a relentless background noise, usually it lasts longer than three to six months—it doesn’t go away quickly and often requires ongoing management strategies even though the injury or illness that caused it has healed or improved.
- Thirdly, neuropathic pain might be more challenge to recognize, as it varies. It can be caused by nerve damage, it presents as burning, shooting, or tingling sensations and requires a particular approach.
- Lastly, nociceptive pain which caused by tissue damage, known for being sharp, aching, or throbbing pain. Although understanding the causes, its management is also not simple.
Acknowledging these pain types is more than academic knowledge, it directly influences treatment plans. If you can surely know the type of pain your patient is suffering, you’re already one step ahead in providing accurate treatment.
By understanding what types of pain your patient is experiencing, you now can tailor your approach. The most important thing is not only which treatment approach you provide to your patient, but also about being effective, efficient, and empathetic in your care.
The Art of Pain Assessment: Tools and Techniques
Every patient is different and the way they experience, or express pain is also not the same. As a beginner nurse, it is vital for you to ask the right questions. Encouraging patients to describe pain in their own words gives you an accurate picture and facilitate the appropriate treatment.
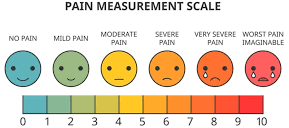
Pain scales are more than just charts on a wall, they’re essential tools in your nursing toolkit. Understanding how to use the Numeric Rating Scale (NRS) from 0 to 10 (0 is no pain and 10 is being the worst), the Wong-Baker FACES Pain Rating Scale can provide quantifiable data to inform treatment decisions. Remember, accuracy is crucial when it comes to evaluating pain level.
Now, what about patients who can’t speak for themselves? This is where observational skills take place. Look for non-verbal signs like grimacing, guarding a body part, or vocalizations. These indicators can be just as telling as a 10 on the NRS, or even more.
Personally, the art of pain assessment is completed only when you integrate your interview technique, knowledge of assessment tools, and the ability to read non-verbal communications. Each piece is paramount in establishing a comprehensive view of the patient’s pain. Once you have mastered this essential skill set, you can prepare to take the next step: pharmacological interventions.
Balancing Pharmaceuticals with Compassion: Safe Medication Practices
As a novice, you start practicing medication administration. It’s pivotal to comprehend the medications commonly used to manage pain, including their doses, routes, side effects, possible interactions and contraindications.
Following the ‘Five Rights‘ of medication administration is not only best practice, but also a responsibility. The ‘Five Rights’ covers identifying the right patient, right medication, right dose, right route, and the right time. These checks prevent you from making errors and a cornerstone of patient safety in medication administration.
Pain management is deeply personal and multifaceted, usually involving opioids and non-opioid analgesics. When giving out opioids, you are responsible for managing risks such as observing for side effects and interactions that could compromise care.
This isn’t just about administering medications, it’s also about being a patient advocate. When patients are in pain, they rely on you not only to manage pain but also to show empathy and pay attention to their individual needs and concerns.
It is so vital to take time to educate your patients about what you are administering, what is the expected outcomes and potential side effects. By doing so, it assists you in establishing the right process when giving medications and can increase your patients’ comfort level as they understand what medications they are receiving. It reinforces the nurse-patient relationship and builds trust.
In my opinion, good pain management considers both physical and emotional states of a patient. You have to balance your clinical knowledge with a compassionate approach. It is essential to remember that patient care is not only about giving medications but also it is about the reassurance and empathy you offer.
Beyond Medication: Integrating Multidisciplinary Pain Relief Strategies

Managing pain isn’t just about the medications—it’s a holistic care. Effective pain relief often requires a combination of approaches, and that’s where non-pharmacological interventions come into place to join with pharmacological interventions. This includes heat/cold therapy, massage, and thoughtful positioning to reduce discomfort. In addition, it doesn’t stop at physical methods; psychological techniques such as relaxation exercises, are powerful weapons in your arsenal against pain.
Now, what’s really important is empowering patients to take an active role in their pain management. When you explain them about how pain works and how to apply these techniques themselves, you’re not just addressing their current pain—you’re proactive to educate them what to do in the future pain.
However, you’re not dealing it by yourself. Effective pain management requires multidisciplinary team, you are working closely with doctors, pharmacists, physical therapists, and even psychologists can make all the difference. By involving into varied expertise, you can craft a pain management plan that is unique to serve a specific patient.
Providing a quality patient care combines documentation and regular reassessment of pain levels and treatment effectiveness. It’s essential to accurately record every assessment, intervention, and patient reaction. Your notes will guide future care and adjustments, ensuring that pain management remains dynamic and responsive.
Your first attempt at managing pain may be a bit daunting, but don’t expect the perfection from the beginning. Pain management is a quickly evolving field, and it’s vital to stay informed about the latest techniques and recommendations. Continuing education workshops and courses is a must as they are opportunities to improve your skills and bring innovative solutions to your patients care.
Choose something that resonates with you and keep building on that knowledge. By integrating these strategies into your practice, you’re going to find a profound sense of accomplishment. You’re not just easing pain; you’re improving lives, and that’s something truly extraordinary in your chosen career.
